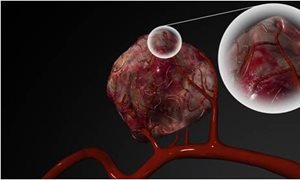
 For the first time Radboud university medical center has treated a patient with liver metastases by using holmium radio-embolization. With this technique, radioactive holmium microspheres are injected via a catheter into the liver artery. These microspheres then become stuck in the small blood vessels of tumors. As a result the tumor is irradiated from close proximity.
For the first time Radboud university medical center has treated a patient with liver metastases by using holmium radio-embolization. With this technique, radioactive holmium microspheres are injected via a catheter into the liver artery. These microspheres then become stuck in the small blood vessels of tumors. As a result the tumor is irradiated from close proximity.
To the clinic
Radboud university medical center is the third medical center in the Netherlands that can offer this treatment with holmium spheres. Frank Nijsen, medical biologist at the department of Radiology and Nuclear Medicine at Radboud university medical center, is pleased with this innovation. More than a year ago he left UMC Utrecht – where he developed the therapy and founded the spin-off Quirem Medical to bring the therapy to the clinic – and joined Radboud university medical center. He wants to use the opportunities at Radboud university medical center to further improve the therapy.
MRI images
Nijsen: “Radboud university medical center has the MITeC, the Medical Innovation and Technology expert Center. This is a collection of innovative surgical facilities; for example, MRI is available in the OR itself. This is important because now we can make MRI images during surgery. This enables us to immediately confirm where the spheres are located and in what concentrations, and to adjust the therapy during the procedure if necessary. For the standard procedure, we do not yet use MRI, but we have submitted a research proposal to optimize radio-embolization with MRI.”
Preparation
Nuclear medicine physician Marcel Janssen, who performed the first procedure with interventional radiologist Mark Arntz and colleagues: “Several weeks before the actual treatment of the patient we already insert a catheter. Afterwards, we determine at what location in the liver artery we can best inject the spheres, we close any ‘leaks’ and we simulate the therapy by injecting soluble protein spheres and observing how they spread. Based on these insights, we decide whether the patient qualifies for the treatment. If all looks well, the patient will be treated 1 or 2 weeks afterwards.”
Improving results
Because real-time MRI imaging is not yet available, adjusting and fine tuning the therapy in individual patients is not yet possible. “We have demonstrated the efficacy of the therapy in previous studies,” says Nijsen. “By using MRI imaging while administering the microspheres, we hypothesize that we can direct the holmium spheres towards the tumor more effectively. We expect this will yield better outcomes, perhaps even with lower dosages. Over the next few years at the MITeC, we will investigate whether this is possible.”
___________________
Quirem Medical, a spin-off of UMC Utrecht, supplies the radioactive micospheres, which are prepared for use by Radboud Translational Medicine. For each treatment, approximately 30 million spheres are used with a diameter of approximately 30 micron. A micron is 0.001 millimeter.
-
Want to know more about these subjects? Click on the buttons below for more news.
Related news items

Take a special look inside Radboudumc on 2 October Open Day for young and old
12 September 2022On Saturday 1 and Sunday 2 October, the Radboud university medical center, Radboud University and the HAN are participating in the 'Weekend van de Wetenschap'. At all locations there are fun and interesting programs for young and old.
go to page
The future of laboratory animal research More attention to living conditions of laboratory animals
16 May 2022 On May 9, a meeting took place at the Radboudumc as a result of the launch of the Dutch Transparency Agreement on Animal Testing. The Radboudumc is one of the twenty signatories and has thus committed itself to openly and transparently communicate its vision and policy with regard to animal testing. go to page
Large NWA ORC grant awarded for national skin research: Next Generation ImmunoDermatology
23 March 2022Research for better treatment methods for chronic skin diseases.
go to page
Thomas van den Heuvel wins Stairway to Impact Award for safer pregnancies using AI Award for safer pregnancies using AI
1 December 2021Radboudumc researcher Thomas van den Heuvel receives the Stairway to Impact Award from Dutch Research Council NWO. He receives this prize for the development of the BabyChecker, a smartphone application that allows midwives to make ultrasounds during pregnancies.
go to page